How to Read Your Medical Bill Correctly
It’s very likely that you won’t look at a medical bill until you get one in the mail addressed to you. When you get around to reading it you may not be able to make sense of what you are reading and why some of the items cost so much.
And if you have spent any time in a hospital recently the bill you get will likely have codes and terms that you have never seen before. But it’s good for you to understand this bill because it could contain costly errors or even intentional overcharging.
Adria Goldman Cross from MedWise Insurance Advocacy says:
Many hospitals know it’s unethical, but it’s not against the law … to charge these outrageous fees, or even bill you for something they didn’t even provide.
If you do end up finding some discrepancies on your bill you can negotiate your medical bill but you better know what you are talking about to get a favorable outcome.
Make sure you have the right bill.
The only way to know if you got billed correctly is to first make sure you have the initial itemized bill in front of you. If you have health insurance you may not be looking at an accurate account of what you owe but it’s still good to see what you were charged for.

Most likely you will get a paper billed physically mailed to you but like the rest of the world everyone is going digital and you should be able to obtain a digital copy of the bill as well. If you are not sure how you can get ahold of the digital copy, reach out to your provider and ask them to send you the explanation of benefits. The particular document will say “not a bill.”
Clerical mistakes are actually quite common. This can be mistakes like name, address, insurance information and dates. All of these small but huge mistakes can really cause issues with an insurance company.
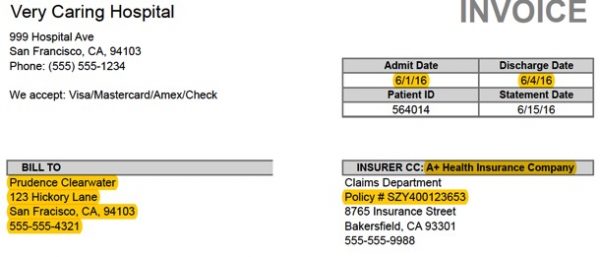
This first bill you should be receiving if you had inpatient or even outpatient care is a summary bill. Usually, the health care provider will send out the summary of charges with a final charge at the end but this doesn’t always happen.
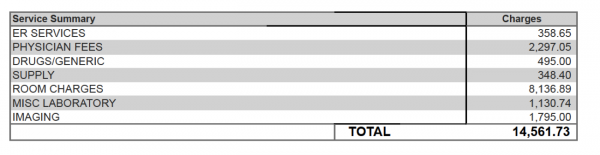
Unfortunately, this is not the bill you need to see what you actually owe. Call the clinic or hospital and specifically ask for the complete, itemized bill for all services you received, with codes. That bill should look something like this:
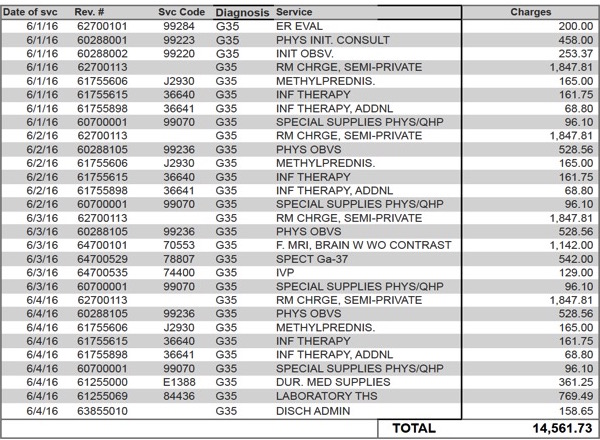
When you get the itemized bill you can start going over it to see if there are any overcharges or mistakes.
Let’s go over those codes.
Before you study that itemized bill you will want to know what some of the codes mean.
 HCPCS Level I, or CPT Codes, are universal, used by all providers in the U.S. and consist of five digits that identify procedures or tests. Often, they are listed as service codes.
HCPCS Level I, or CPT Codes, are universal, used by all providers in the U.S. and consist of five digits that identify procedures or tests. Often, they are listed as service codes.
![]()
HCPCS Level II Codes these usually indicate supplies that were used during your visit. They usually start with a letter, rather than a number, but are also referred to as service codes.
ICD-10 Codes are a system to identify every possible diagnosis. ICD codes are from the International Classification of Diseases, and in the U.S., every billed service with a CPT code must also be linked to an ICD code to assure the treatment fits the diagnosis. If you only have one condition being treated at the visit, all of the diagnosis codes should be the same, or start the same.

Revenue codes identify the dollar amount associated with the procedure and are specific to each facility, so there aren’t universal revenue codes.
Any of these codes could show up on your explanation of benefits or your health insurance summary of charges.
Do some research.
Open your internet browser and do a little research.
- A medical dictionary to help you understand any medical terms.
- An HCPCS or CPT Code reference. The most reliable tool may be the Medicare code lookup, but be sure to ignore the pricing information at the bottom unless you are an actual Medicare beneficiary, since Medicare’s set prices are generally well below what everyone else pays. Once you accept the user agreement, you’ll be taken to a page with several options; don’t adjust any except the drop-down “Modifier” menu at the bottom, where you’ll select “All Modifiers.” Right above that is where you can enter your codes.
- An ICD code reference will also help, just to make sure you’re being billed for the correct diagnosis. Sometimes, providers will alter diagnosis codes so they can bill for a more expensive procedure, Gross says.
At the end of the day, it’s your responsibility to understand your medical bills and ensure that you are not being overcharged. Take the time to learn a little bit about what you were billed for.

Add Comment